Marijuana and Older adults: So Many Burning Questions
Author(s):
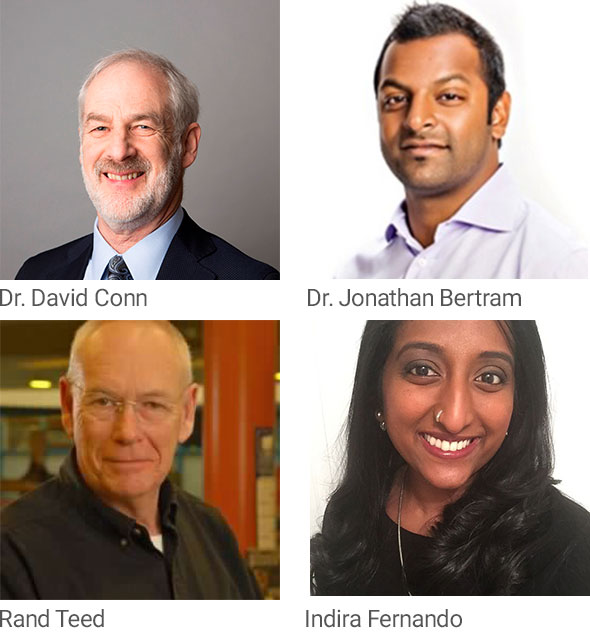
Dr. David Conn
Canadian Coalition for Seniors’ Mental Health
Co-Chair
Dr. Jonathan Bertram
Cannabis Use Disorder Working Group at the Canadian Coalition for Seniors’ Mental Health
Co-Chair
Rand Teed
Canadian Coalition for Seniors’ Mental Health
Canadian Certified Addiction Counsellor-Member of the Cannabis Use Disorder Working Group
Indira Fernando
Canadian Coalition for Seniors’ Mental Health
Project Coordinator
The legalization of Cannabis steadfastly approaches our nation this fall. Canada stands out as the first of the G7 countries to adopt such a monumental policy change in its drug legislation. The magnitude of this event will be felt for many years to come and will have profound effects on our economy, health care, education and policy systems. The effect on the overall lifestyle and well-being of Canadians is a reminder that our substance use landscape is at a very critical junction. While much of the discourse that surrounds cannabis has been focused on youth; a unique population to consider is that of older adults. Older adults face a variety of health problems and are a particularly vulnerable and often stigmatized group. The rise of medical cannabis use in the midst of pending legalization for recreational use presents the Canadian science and policy environment with new opportunities as well as challenges for consideration.
We now see many baby boomers who grew up during the “hippy” years reaching well into their 60s and 70s. They are increasingly using cannabis for a variety of medical reasons including pain management. Recent Canadian guidelines for Family Physicians recommend only four conditions for which cannabis might be worth considering, which contrasts significantly from usual practice in cannabis medical clinics. An increasing number of older adults comprise this key market area, and it brings to attention the need for increased awareness and education around the benefits and risks of being a consumer.
The industry has done an excellent job often marketing cannabis as an effective “cure-all”, primarily driven by economics and politics rather than health. It will be important to evaluate how the motivation for the medical use of cannabis will interact with consumption of recreational cannabis. There is a lack of foundation to support the evidence base versus anecdotal support for the therapeutic effects of cannabis.
The medical conditions pertinent to aging also add a layer of complexity when considering cannabis use for older adults. Older adults experience changes in physiology and some have greater intake of medications due to co-morbid conditions. As a result much is still unknown about the pharmacological interactions of cannabis use and its overall effect on health issues seen in later life. An example of an area of caution is the increased risk of falls or the effect on mobility and cognition faced by older cannabis users. The increased availability, reduced risk perception and easier access that follow legalization may mean that more seniors will consider the usage of this drug without sufficient knowledge in hand.
As the percentage of Ontarians over 50 who used cannabis in the past year nearly tripled over the last 10 years, and rose fivefold since 1977, concerns that arise include whether clinicians, researchers and policymakers alike are able to keep up with the growing need for further knowledge over the upcoming months. The indications for recreational and medicinal use are emerging together in a fashion that is unique for older adults and we are in much need of collaborative evidence building.
In light of these changing times a new initiative currently being developed by the Canadian Coalition for Seniors’ Mental Health are guidelines for substance use disorders in older adults. In the fall of 2018 the Coalition aims to release four documents covering benzodiazapine, alcohol, opioids and cannabis use disorders. The guidelines are intentional in being evidence-based, broad in scope and reflective of the continuum of settings for care. With the inclusion of the lived experiences of consumers, the guidelines project aims to take account of both the cultural diversity as well as psycho-social factors that guide decision making when considering cannabis use.
In all things, it is what we think that determines how we act. Cannabis products have changed significantly since today’s seniors were in their teens and 20s. There are different strains and most importantly the primary psychoactive cannabinoid THC is much stronger in some strains. Secondly, the ratio of THC to CBD has changed making this drug considerably different than in the past. If we think this a “soft” drug with few side effects other than the intake of more potato chips then it will not get treated with the care and respect it deserves. As a result , we need to help health professionals and older adults acquire a sufficient knowledge base to move cautiously into this new world.
Allan, GM et al. (2018) Simplified guideline for prescribing medical cannabinoids in primary care. Canadian Family Physician 64: 111-120.
Alomiteanu AR, Hamilton H, Adlaf E, Mann RE. CAMH Monitor eReport 2015: Substance use, Mental Health and Well-being among Ontario Adults. Toronto, Ontario: Centre for Addiction and Mental Health; 2016
Fischer, B., Russell, C., Sabioni, P., van den Brink, W., Le Foll, B., Hall, W., Rehm, J. & Room, R. (2017). Lower-Risk Cannabis Use Guidelines (LRCUG): An evidence-based update. American Journal of Public Health, 107(8).
Kara L. Martin, Leigh Blizzard, Velandai K. Srikanth, Amanda Wood, Russell Thomson, Lauren M. Sanders, Michele L. Callisaya; Cognitive Function Modifies the Effect of Physiological Function on the Risk of Multiple Falls—A Population-Based Study, The Journals of Gerontology: Series A, Volume 68, Issue 9, 1 September 2013, Pages 1091–1097
Russo, E. B. (2008). Cannabinoids in the management of difficult to treat pain. Therapeutics and Clinical Risk Management, 4(1), 245–259.

